Basic Medical Terms
Illness Terminology
Cavernous Malformations (CCM, cavmal), Cavernoma, and Cavernous Angioma are terms often used interchangeably to describe mulberry-shaped abnormal blood vessels in the brain or spinal cord. These terms refer to both the lesion itself and the medical condition.
Acute
Having a sudden onset
Lesion
Any abnormal or injured tissue. A cavernous malformation is a lesion.
Overt
Not contained. Hemorrhages that bleed outside of the cavernous malformation into the surrounding brain tissue are considered overt.
Stochastic
Occurring by chance.
Tissue
A group of cells that are united to perform the same function.
Tumor
New growth of tissue in which multiplication of cells is uncontrolled and progressive. When a tumor is benign, cell multiplication within the tumor is minimal. The benign tumor does not “spread” or cause the growth of new tumors in other areas. Cavernous malformations have been considered benign tumors by some researchers. Recent evidence suggests that cavernous malformations develop initially like tumors; then, they grow further as they bleed.
Blood and Blood Vessel Terminology
Artery
A blood vessel through which blood passes away from the heart and into other parts of the body. Blood flows through arteries with a great deal of pressure resulting from the pumping action of the heart. A pulse can be heard and felt in an artery. When arteries are ruptured, they bleed profusely. Cavernous malformations do not involve arteries. As arteries reach their destinations, they branch and become much smaller vessels called arterioles.
Capillary
Tiny vessels that connect the arterioles and venules. Capillaries have a very controlled flow, allowing for the exchange of oxygen and nutrients between blood vessels and the surrounding tissue. Some researchers believe that some cavernous malformations begin as abnormal capillaries.
Circulation
Endothelial
The layer of cells that lines the blood vessels and other organs. Cavernous malformations are comprised of endothelial cells that lack the support of the outer layers of the blood vessel. The lack of support makes them leaky and fragile. Mutations, or errors in the gene coding in the endothelial layer, are what cause cavernous malformations.
Hemorrhage
The escape of blood from the vessels. Cavernous malformations exhibit three types of hemorrhage:
- Cavernous malformations can bleed slowly within the walls of the angioma and remain quite small. A small hemorrhage may not require surgery but may reabsorb into the body. However, continued small bleeds in the same cavernous malformation often cause deterioration in function.
- Cavernous malformations can bleed more profusely within the walls of the angioma. The bleeding can cause them to grow and put pressure on the surrounding brain tissue.
- Finally, cavernous malformations may bleed through a weak spot in the angioma wall into the surrounding brain tissue. This release of blood is called an overt hemorrhage.
Hemosiderin
An iron deposit which is a blood breakdown product
A hemosiderin ring surrounds all cavernous malformations. A hemosiderin ring is visible on MRI and means that the cavernous malformation has leaked or bled sometime in the past. Hemosiderin can irritate brain tissue and may be the cause of some seizures.
Thrombosis
The formation of a blood clot along the wall of a blood vessel. The clot reduces or cuts off blood flow into the area beyond. A clot also forms after blood leaks from a blood vessel.
Vein
One of the vessels that carry blood from the capillaries back to the heart. Blood traveling through veins moves with much less pressure than blood going through arteries. Veins begin as venules, small veins, and combine to form veins as they get closer to the heart.
Parts of the Brain
Brainstem
The part of the brain that connects the cerebral hemispheres with the spinal cord. The brainstem consists of several structures, including the pons, medulla oblongata, and mid-brain, which consists of the reticular formation, raphe nucleus, substantia nigra. Some people also include the structures of the diencephalon (thalamus, pineal gland, habenula, caudate and lenticular nuclei, and hypothalamus) as part of the brainstem. These structures are responsible for the most basic life functions.
Cerebellum
The part of the brain that lies between the brainstem and the back of the skull. It is primarily concerned with the coordination of movement.
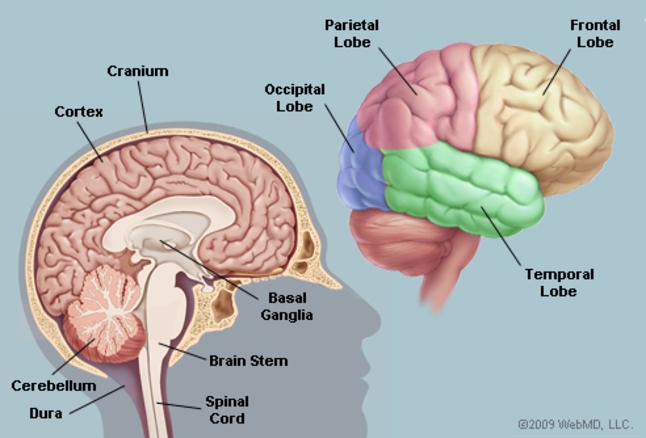
Cerebrum
The portion of the brain that occupies the upper part of the skull. It is divided into two hemispheres, which are connected by the corpus callosum. The cerebrum forms the most substantial portion of the human central nervous system. Each half of the cerebrum contains four sections or lobes. They are the frontal lobe, the parietal lobe, the temporal lobe, and the occipital lobe. Below the cerebrum are the structures of the cerebellum and brainstem.
Cerebral Cortex
The outer layer of the cerebrum. The cerebral cortex is the 3 mm layer of gray substance covering the surface of each cerebral hemisphere.
Dura Mater
The outermost, toughest, and most fibrous of the three membranes that cover the brain and spinal cord.
Epidural or Extradural
Outside of the dura mater. For cavernous malformations, this term is used for a rare condition in which there are lesions between the spinal cord and vertebra.
Gray Matter
This term is most commonly used as another name for the tissue of the cerebral cortex, which makes up the outer layer of the brain. This tissue is colored gray. Although other areas of the brain are also gray, such as the thalamus, they are usually not included when medical or laypeople use this term.
Infratentorial
Below the level of the tentorium of the cerebellum. The tentorium is a layer of dura mater that supports the occipital lobes and covers the cerebellum. The cerebellum, pons, medulla, midbrain, and fourth ventricle lie below this layer and are considered infratentorial. About 27% of cavernous malformations are infratentorial. [1]
Intramedullary
Most interior portions of the brain or spinal cord. This term is most often used when referring to cavernous malformations of the spinal cord.
Meninges
The three membranes that envelop the brain and spinal cord: the dura mater, pia mater, and arachnoid.
Subarachnoid
Below the level of the arachnoid layer. In other words, below the level of the meninges of the brain.
Supratentorial
Above the level of the tentorium, which is a layer of dura mater, that supports the occipital lobes and covers the cerebellum. The cerebral hemispheres, thalamus, basal ganglia, lateral and third ventricles, and hypothalamus lie above this level and are considered supratentorial. About 73% of cavernous malformations are supratentorial. [2]
White Matter
Another name for the tissue located in the interior of the brain. This tissue is white. It is located under the cerebral cortex, which is colored gray.
Genetics of Cavernous Angioma
A more complete discussion is on our Genetics of Cavernous Angioma page.
CCM1
The CCM1 gene codes for the production of a protein called Krev Interaction Trapped 1 (KRIT1). KRIT1 protein works in complex with the CCM2 and CCM3 gene products as well as other partners to maintain tight connections between neighboring blood vessel cells. Mutations that destroy the function of KRIT1 result in the onset of cavernous malformation.
CCM2
The CCM2 gene codes for the production of a protein called malcavernin. Malcavernin is a scaffolding protein – its function is to bring together and support protein complexes. Mutations that cause a loss of function for malcavernin result in the onset of cavernous malformation.
CCM3
The CCM3 gene codes for the production of the Programmed Cell Death 10 protein (PDCD10). Originally named for its function related to apoptosis (a controlled cell death process), PDCD10 is also involved in many signaling processes related to blood vessels and maintaining proper junctions between neighboring blood vessel cells. Loss of function mutation of CCM3 results in the most aggressive form of cavernous malformation.
Familial cavernous malformation
Approximately 20% of cavernous malformation cases are familial. Familial cavernous malformation is caused by the inheritance of a mutation to one of three genes, CCM1, CCM2, or CCM3. Familial cavernous malformation is an autosomal dominant disorder, which means that it does not skip generations within affected families. Additionally, each affected person has a 50% chance of passing the illness to each of his/her children. Individuals with familial cavernous malformation typically develop multiple lesions over time.
Sporadic cavernous malformation
Sporadic cavernous malformation accounts for about 80% of all cases. In comparison to the familial form of the illness, sporadic cavernous malformation is not caused by an inherited mutation, does not run in families, and affected individuals typically develop only a single lesion.
Developmental venous anomaly (DVA)
A DVA is typically an abnormal vein, which is benign and carries no serious risk as long as it remains unchanged on repeated MRI scans, and is not associated with microbleeds. When it is associated with bleeding, this is caused by a solitary or sporadic cavernous malformation that grows on the branches of the DVA, like a berry on a tree. When a cavernoma is resected (see below), it is important not to injure the DVA, which is needed to drain blood from the normal brain.
Radiation-induced cavernous malformation
Radiation to the brain is another potential cause of cavernous malformation lesion development, sometimes resulting in multiple lesions clustered together in sporadic cases, where solitary lesions are typical. Because of the potential for new lesion development, radiosurgery is not a recommended treatment option for familial cavernous malformation.
Cavernous MALFORMATION Life Cycle
Calcification
The process by which tissue becomes hard by a deposit of calcium salts within the tissue.
De Novo Lesion
A cavernous malformation that was not present at birth. Developing de novo lesions is a hallmark of familial cavernous malformation. It may also occur as the result of the presence of a developmental venous anomaly (DVA) or radiation used to treat brain or spinal cancer.
Stage I
A cavernous malformation lesion in the earliest stages of development. Typically, this is a single dilated cavern and only visualized at the highest field MRI technologies.
Stage II
A multi-cavernous lesion (with multiple dilated blood vessels). These are mature lesions, often prone to hemorrhage, and readily visualized with MRI.
Disability-Related Terminology
Assistive Technology
Computer software and hardware devices that allow individuals with physical limitations to use the computer and other household and work environment equipment. For example, speech assistive technology can allow an individual with hand or arm limitations to use their voice to control his or her computer.
Rankin Scale
The Modified Rankin disability scale measures the degree of disability an individual has. Several research studies make use of this scale. There are five grades:
- Grade 0 – none or almost none
- Grade 1 – slight. A person may not be able to do all of the things she could previously do, but she can take care of herself.
- Grade 2 – moderate. A person requires some adjustments in daily living but can do the essentials without the help of another person. For example, he may need a cane to walk or may be unable to drive.
- Grade 3 – moderate-severe. A person requires another person’s help to take care of herself. She may need help dressing or bathing. She can not walk without someone’s assistance.
- Grade 4 – severe. A person requires constant nursing care because he is bedridden. He is likely to be incontinent.
- Grade 5 – death.
Imaging
A complete discussion is available on our Imaging page.
Angiographically Occult
A description of vascular malformations that can not be seen on an angiogram. Cavernous malformations are angiographically occult because blood flow through the lesion is low. Angiography is not used for cavernous malformation unless there is concern about a misdiagnosis.
Computerized Axial Tomography (CAT or CT scan)
An x-ray technique that produces pictures of consecutive slices of a body part. Cavernous malformations can be seen using a CAT scan, but are often difficult to distinguish from other types of tumors. The slices of the CT scan may not be close enough to detect all of the cavernous malformations a person might have. CT is useful for gross visualization of a large cavernous malformation, e.g., to track growth.
Contrast
A process in which gadolinium dye is injected into a person’s bloodstream during an MRI to increase the contrast between light and dark areas.
Gradient Echo Sequences (GRE)
GRE is a type of magnetic resonance imaging that is very accurate in detecting cavernous malformations. A more precise, technical definition can be found at the FONAR MRI glossary
Magnetic Resonance Angiography
A form of magnetic resonance imaging (see MRI below) used to study blood vessels and blood flow. MRA is used to differentiate cavernous malformations from other types of vascular abnormalities.
Magnetic Resonance Imaging
A method of imaging soft tissues of the body, such as the brain and spinal cord, by applying an external magnetic field. Magnetic resonance images distinguish between hydrogen atoms in different environments and produce a picture of these environments.
Susceptibility Weighted Imaging (SWI)
SWI is a type of magnetic resonance imaging that is very accurate in detecting the tiniest cavernous malformations that can be seen in humans. For those with the hereditary form of the illness. susceptibility-weighted imaging (SWI) sequences will typically show twice as many lesions as gradient-echo sequences. Additional lesions do not mean that a patient has developed new lesions but rather that the imaging technique is more sensitive.
Quantitative Susceptibility Mapping (QSM)
QSM is a new MRI technique that measures iron content (a surrogate measure for the amount of blood leak) and is being developed as a biomarker of disease activity. It is available only in specialized research centers and is not currently used for clinical decision-making.
Other Types of Vascular Malformations
Arterio-Venous Malformation (AVM)
A vascular abnormality in which arteries and veins have a direct connection (shunt) rather than having blood flow through a bed of capillaries. AVM’s are high flow malformations.
Capillary Telangiectasia
Capillary telangiectasias are tiny lesions composed of dilated capillaries. They have no symptoms. Some researchers believe that these malformations can develop into cavernous malformations.
Developmental Venous Anomaly (DVA)
Also known as venous angioma. Developmental venous anomalies consist of one or more abnormal veins, often in the deep white matter of the brain. Most commonly, small veins that originate in the most interior parts of the brain are arranged in a fan shape and drain toward the outer portions of the brain into one or more dilated draining veins. These draining veins then drain out toward the cortex. There is normal brain tissue between the veins, and no arteries are found associated with the developmental venous anomaly. Most often, developmental venous anomalies have no symptoms. Very rarely, they exhibit calcification, hemorrhage, or spontaneous thrombosis, or they may cause headaches. They are believed to be found in 1 in 50 people. DVAs are often associated with cavernous malformations, particularly in people who have a solitary cavernous malformation, and they likely play a role in the development of sporadic cavernous malformations.
Seizure
A complete discussion is available on our Seizure page and the Epilepsy Action website.
Focal Seizure
A focal seizure, also known as a focal onset seizure, starts in one area of the brain. A focal seizure is the typical seizure found with cavernous malformation since seizures usually originate near a lesion. There are two types of focal seizure: focal aware and focal impaired awareness. Each of these can be primarily motor or non-motor.
Focal Aware Seizure
Formerly called a simple partial seizure, in a focal aware seizure, the person stays aware of what is happening around them. They are unable to stop their experience or behavior. The seizure behavior depends on the area of the brain affected. The seizure can result in such things as intense feelings, uncontrolled movements, vision problems, or speech problems.
Focal Impaired Awareness Seizure
Formerly called complex partial seizures, in a focal impaired awareness seizure, there is a loss of awareness, and the person engages in “automatisms” – behaviors such as chewing, swallowing, picking at clothes, or scratching.
Motor versus Non-motor seizure
In motor seizures, the activity during a seizure primarily involves movement like jerking or twitching. In non-motor seizures, the person experiences changes in emotions, thinking, or sensations. Both are focal seizures.
Generalized Onset Seizure
Generalized seizures involve both sides of the brain from the start. A focal seizure can sometimes generalize to other areas of the brain, but this is not the same as a generalized onset seizure. Absence seizures and most tonic-clonic seizures are generalized onset seizures. Tonic, myoclonic, and atonic seizures can be either generalized onset or focal onset.
Absence
Also known as a “stop and stare” seizure. The person having the seizure stops what they are doing and blankly stares into space. The person is not aware that they have had a temporary interruption of their activity.
Tonic-Clonic
Formerly known as “grand mal.” A tonic-clonic seizure is the classic representation of a seizure and usually involves the entire brain from the onset. During a tonic-clonic seizure, a person loses consciousness, falls to the ground, and may stop breathing for a short period. They may have a period of jerky limb movements, after which they go limp but remain unconscious. Gradually, the person regains consciousness and will likely feel very tired.
Myoclonic
Myoclonic seizures, also known as myoclonic jerks, are brief twitches or spasms that can involve all or part of the body.
Traditional Surgery
A more complete discussion can be found in our Surgery section.
Craniectomy
A surgical procedure in which a portion of the skull is removed to access the brain.
Craniotomy
A surgical procedure in which the skull is opened to access the brain.
Image-Guided Surgical Navigation: Computer-Assisted Stereotaxy, Frameless Stereotaxy
These are techniques in which imaging, such as MRI, is used during surgery to precisely locate a cavernous malformation. It allows for more precision in removing the cavernous malformation and may eventually reduce the invasiveness of cavernous malformation resection.
Resection
Surgical removal of a cavernous malformation or other mass. Resection is usually done with computerized image guidance (described above) and with the operating microscope. Resection is usually performed while monitoring the electrical function of the brain to minimize injury to the normal brain.
Other Surgical Techniques
A more complete discussion can be found on our Minimally Invasive/Non-invasive Surgery page.
Stereotactic Laser Ablation
Stereotactic laser ablation is also known as magnetic resonance (MR) thermography-guided laser interstitial thermal therapy (LITT). It is a technique in which a small opening is made in the skull to insert a laser device into the brain. SLA uses real-time MR thermography to coagulate tissue at 50–90°C (122-194°F) while allowing the surgeon to see the nearby structures that need to be protected. Most often, LITT is used to treat lesions that are causing epilepsy, but it is not used to treat or prevent cavernous malformation bleeding.
Stereotactic Radiosurgery (SRS)
Focused radiation aimed at scarring cavernous malformations, while limiting radiation exposure to healthy brain tissue. SRS is considered when a lesion has caused bleeding but cannot be resected safely. The SRS is performed with a variety of radiation instruments, including Gamma Knife, Cyberknife, and linear accelerator (LINAC). It uses advanced tools such as shaped beam, modulated beams, and microleaf collimators, to help guide the radiation more precisely. SRS may cause serious complications, and does not eliminate the lesion. Even the slightest leak of radiation from SRS may cause new lesion formation in familial CCM cases, so it should not be used in that setting.
References
[1] Hsu, FPK, Rigamonti, D, and Huhn, SL. Epidemiology of cavernous malformations. In Cavernous Malformations, Awad IA and Barrow DL eds., Park Ridge, IL: AANS, 1993.
[2] Ibid.
General References
Awad, IA, and Barrow, DL. eds., Cavernous Malformations, Park Ridge, IL: AANS, 1993.
Dorland’s Illustrated Medical Dictionary, 29th edition
This page was last updated 4.16.2022


