Printable PDF versions of this page about cavernous malformation are available in English, Spanish, and Portuguese.
If you are a medical professional and would like printed copies in booklet format, please contact us at info@alliancetocure.org.
1) What is Cavernous Malformation?
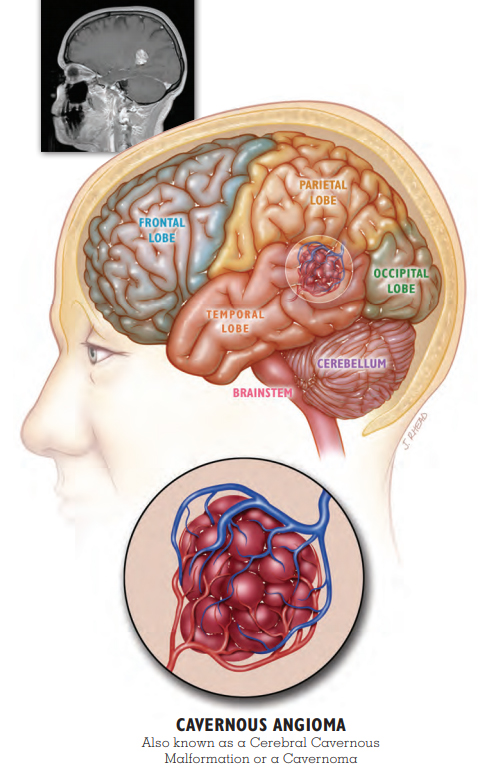
Cavernous malformations are also known as cavernous angioma, CCM, and cavernoma. They are made of abnormal blood vessels. They are not cancerous. Cavernous malformations are made of the smallest blood vessels, called capillaries. They resemble mulberries and have very thin walls compared with other blood vessels. Blood moves through them very slowly. The thin vessel walls can be leaky, allowing blood into the surrounding brain or spinal cord tissue. We believe about one in every 500 people has a cavernous malformation, but most people never have symptoms. Of the people who have a cavernous malformation, we believe many will never have a symptomatic hemorrhage.
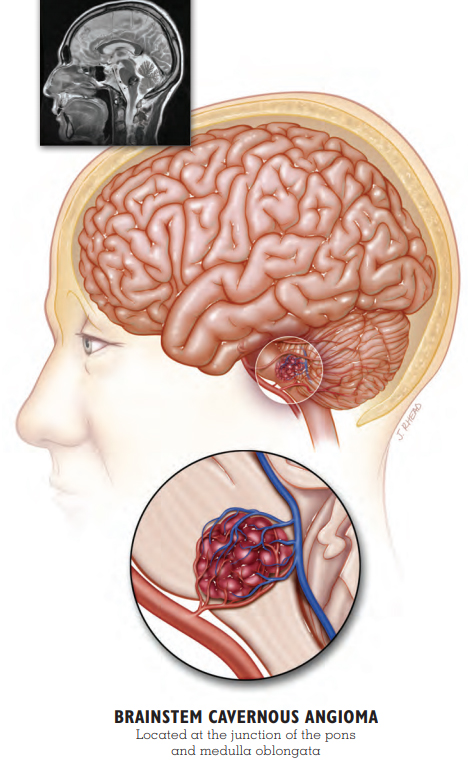
The rarest place for a symptomatic cavernous malformation is in the spinal cord. A spinal cord cavernous malformation is not the same as a spinal hemangioma, which is located in the vertebra (bone). Cavernous malformations may also occur in the area of the brain called the brainstem. Spinal cord and brainstem cavernous malformations can cause more severe symptoms when they hemorrhage.
 Patient Story: Stacie
Patient Story: Stacie
Sporadic Cavernous Malformation with Seizure
Stacie awakened in the middle of the night, just like many other nights. Only this time, as she tried to walk across the room, she became unsteady and fell into the wall. The dizziness happened again the next morning. A 36-year-old mother of four, Stacie sought medical help, but after numerous tests, the doctors were unable to provide her with a diagnosis.
One evening a year later, Stacie experienced what she later would learn was a series of partial complex seizures that included involuntary movement, a loss of awareness, and difficulty speaking. Her husband rushed her to the local hospital where a CT scan revealed an unidentified mass deep in her right temporal lobe. Stacie transferred to a larger hospital with more advanced diagnostic capabilities where she received an MRI.
Her brain mass was diagnosed as a cavernous malformation (cavernous angioma, cavernoma), and she was discharged on anti-seizure medication. Despite this, the seizures continued, and she sought a surgical consultation. The doctors informed her that removing her lesion would be difficult because of its deep location, and surgery could cause additional harm. Stacie needed to accept her new normal.
It has been a year since her diagnosis. After trying a few different anti-seizure medications to find the best fit, Stacie’s seizures are now under control. She says she has learned to leave her high heels in the closet because she still experiences dizziness. Sometimes she has trouble finding the right words. “It’s like playing charades with my kids,” laughs Stacie. “Eventually they figure out what I mean.” She is happy to be driving again and to be able to take care of her family.
Says Stacie, “My brain hemorrhage changed my life, but I know there’s a reason. I will use it as a strength and not a weakness.”
2) WHAT IS AN INCIDENTAL CAVERNOUS malformation?
Your doctor may have discovered your cavernous malformation (cavernous angioma, cavernoma) when you had brain or spinal imaging for a reason not related to your cavernous malformation. For example, you may have received a CT scan or an MRI after a car accident or concussion. In this case, doctors will call your cavernous malformation an incidental finding. Research has shown that incidental cavernous malformations that have not had a previous hemorrhage have a very small chance of ever becoming problematic. While you may want to follow the precautions listed in the Hemorrhage section of this booklet, you may not need repeat imaging unless instructed by your doctor or you develop symptoms. However, many doctors and patients choose to have imaging, typically with MRI, to monitor the lesion. For example, your doctor may order imaging during pregnancy, after medication changes, if another illness is diagnosed, or at times of dramatic lifestyle change, which can include extreme or unusual exercise.
3) WHO MIGHT BE INVOLVED IN MY CARE?
- NEUROLOGIST – manages symptoms like seizure and pain
- NEUROSURGEON – evaluates for surgery
- REHABILITATION SPECIALISTS – improve functioning after brain event
- ORTHOPEDIST – monitors spine in CCM3 patients (see Genetics)
- NEURO-OPHTHALMOLOGIST – cares for brain-related vision problems
- GENETICIST – evaluates for the hereditary form of the illness
- DERMATOLOGIST – cares for vascular skin lesions in hereditary illness
4) WHAT CAUSES MULTIPLE CAVERNOUS malformationS?
Some people have more than one cavernous malformation (cavernous angioma, cavernoma). This can happen for several reasons:
- Most commonly, people with more than one cavernous malformation have a hereditary form of the illness. People with the genetic form of the illness typically develop additional cavernous malformations over time.
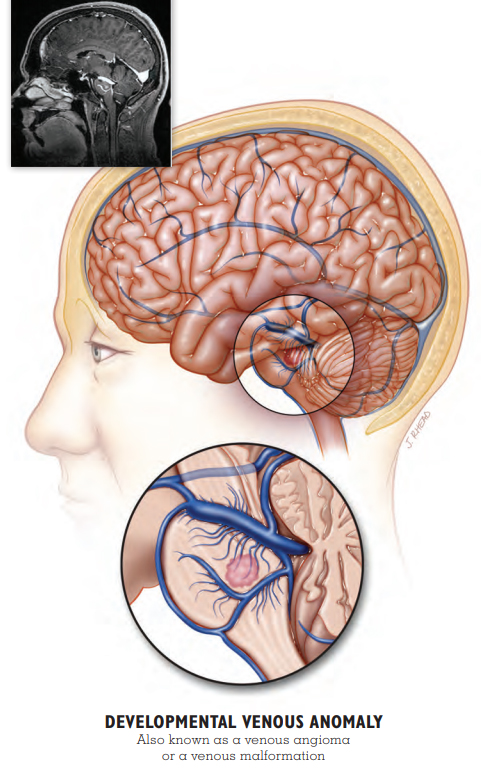
- Some people may have a second kind of abnormal blood vessel called a developmental venous anomaly (DVA). Your doctor might also call this a venous malformation or venous angioma. This dilated blood vessel only rarely causes symptoms on its own. However, it may create conditions that make it more likely for cavernous malformations to form. This is not hereditary.
- Brain or spinal radiation for cancer treatment can cause cavernous malformations to form many years later. In people with the hereditary form, radiosurgery to treat a cavernous malformation may also cause more lesions to form. You can find more information about radiosurgery in the section on Other Treatments.
5) WHAT IS SPORADIC CAVERNOUS Malformation (Cavernous angioma, cavernoma)?
Sporadic cavernous malformation means that you are the only one in your family to have a cavernous malformation, and you do not have a genetic mutation that would cause your children to inherit the illness. Usually, individuals with the sporadic form of the illness have just one cavernous malformation with no other visible blood vessel abnormalities or medical history to explain the lesion.
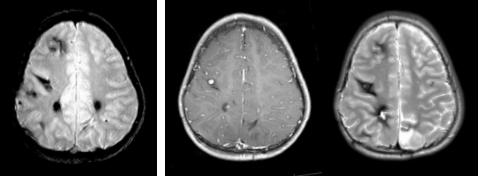
Sometimes, individuals have a different kind of blood vessel abnormality called a developmental venous anomaly (DVA) or they have a history of brain radiation for cancer. A DVA or brain radiation can lead to the development of one or more cavernous malformations (see What Causes Multiple Cavernous Malformation? above). To be certain you have the sporadic form of the illness, you will need to have an MRI with some special images called susceptibility-weighted imaging or SWI. Ask your doctor if this was part of your original MRI. See Stacie and Vern’s Patient Stories to learn more about sporadic cavernous malformation with and without a DVA.
6) WHAT IS A BLEED OR HEMORRHAGE?
All cavernous malformations (cavernous malformations, cavernomas) have some chronic oozing of blood in the area of the lesion. This is what gives their typical appearance on MRI. Oozing is different from the more significant hemorrhage or bleed. A hemorrhage is new bleeding in the cavernous malformation and is often associated with new symptoms. Symptomatic hemorrhage is the most serious complication of cavernous malformation and is the most common reason for surgery. The hemorrhage may cause new symptoms or an increase in symptoms. The specific symptoms a person experiences will depend on the location and size of the cavernous malformation and the amount of blood that has leaked outside the lesion. Eventually, the blood breaks down leaving behind an iron deposit called hemosiderin.
Most lesions never hemorrhage. However, once a cavernous malformation has had one hemorrhage, it is at a significantly greater risk of bleeding again. In the first five years after a hemorrhage, the risk of another hemorrhage in a cavernous malformation that is not in the brainstem is 17-20% (1 in 5 lesions will have a second hemorrhage). The risk of a second hemorrhage in brainstem cavernous malformations is greater at 30% (1 in 3 lesions will have a second hemorrhage). Most of these second hemorrhages will take place in the first two years after the original hemorrhage. Fortunately, five years after a hemorrhage, the risk of another hemorrhage gradually returns to a rate that is similar to the risk from a lesion that has never bled.
 Patient Story: Taylor
Patient Story: Taylor
Brainstem Cavernous Malformation
In January 2015, three-year-old Taylor’s parents, Elizabeth and Pasco, grew concerned when they noticed changes in their daughter’s behavior. Taylor’s walking was unsteady, her speech was impaired, and her face was drooping. MRI confirmed that Taylor had a large cavernous malformation that had hemorrhaged in the pons region of her brainstem.
Taylor’s parents faced a difficult decision. Surgically removing the cavernous malformation could result in additional deficits. However, another hemorrhage could be life-threatening. Elizabeth and Pasco obtained multiple surgical opinions and decided to move forward with surgery at a hospital on the other side of the country. Nine months after the onset of her symptoms, Taylor underwent the delicate operation.
Taylor emerged from the surgery with left-sided facial paralysis, not uncommon with trauma to the pons. She had difficulty coordinating her movements, which affected her standing and walking. Since her surgery, Taylor has undergone intensive physical rehabilitation and made great improvements in her ability to get around. Her family is researching options to bring movement back to her face.
Because she had additional cavernous malformations, Taylor received genetic testing. Testing revealed a mutation of the CCM3 gene, which tends to lead to a more severe form of cavernous malformation illness. Taylor is the first in her family to have a CCM3 mutation.
Taylor’s parents are grateful for the positive surgical outcome, but they still worry. “Unfortunately, always in the back of mine and her daddy’s mind is the anxiety of not knowing what is going on in there,” said Elizabeth. “Is there any new activity, anything we should know about?”
Elizabeth and Pasco treasure Taylor and her resilience. “She is beautiful, smart, charming, witty, stubborn, and strong. She still amazes us every day with things she does.”
7) WHAT CAUSES HEMORRHAGE?
We do not know what causes hemorrhage. Without evidence, it is hard for doctors to recommend specific precautions.
- People with multiple cavernous malformations, usually caused by a familial form of the illness, are at higher risk.
- There is no evidence at this time that medications or supplements that thin blood, such as ibuprofen or aspirin, can cause hemorrhage. However, doctors may recommend limiting their use. It is also not clear whether hormonal birth control or estrogen supplements should be restricted, but some doctors advise this, especially if a patient had a prior bleed on such medications or while pregnant.
- Behaviors that can increase inflammation like smoking cigarettes may increase the risk of hemorrhage.
- There is no reason to avoid flying in airplanes.
- This is no reason to reduce aerobic exercise. We do not have enough data to determine whether weight-lifting may place one at higher risk.
- Researchers don’t know if head trauma, including that which you might experience with contact sports, can cause hemorrhage.
Things you can do:
- Animal studies have shown that MAINTAINING NORMAL VITAMIN D levels may be protective. Clinical research has indicated that patients who are Vitamin D deficient are more likely to have had active lesions. Your doctor can check your Vitamin D level with a blood test.
- PROTECT YOURSELF against preventable, contagious illnesses with hand washing, and vaccinations.
- FOLLOW YOUR DOCTOR’S ORDERS to manage other chronic illnesses, such as high blood pressure and diabetes.
8) WHAT SYMPTOMS CAN A CAVERNOUS malformation CAUSE?
- Seizures are one of the most common symptoms of cavernous malformation (cavernous angioma, cavernoma). Seizures fall into two general groups: focal seizures that are local to one area of the brain and generalized seizures that involve both sides of the brain. All cavernous malformation seizures begin as focal seizures but some progress to generalized seizures. Neurologists use anti-epilepsy medications to control seizures. However, neurosurgeons have had good results in eliminating seizures with brain surgery if they are able to pinpoint which cavernous malformation is causing the seizures. Surgery is most successful when it occurs within two years of a first seizure. Brainstem and spinal cavernous malformations do not cause seizures.
- We know people with cavernous malformation experience more frequent headaches than other people. A headache does not necessarily mean a new hemorrhage. For the most part, we can’t distinguish a cavernous malformation headache from any other kind of headache. A headache unlike one you have ever experienced or headaches, particularly on the same side or general location as your lesion, may be related to your lesion. A headache may be related to your cavernous malformation if it is unlike one you have ever experienced or if it is in the general location of your lesion.
- The symptoms of a cavernous malformation hemorrhage depend on its location and size. Cavernous malformations can cause attention, memory, social skills, mood, and learning problems, particularly if the lesions are in the frontal, parietal, or temporal lobes, or in the cerebellum, even without obvious bleeding. This is particularly true for individuals with many lesions throughout the brain.
- Cavernous malformations in many parts of the brain and spinal cord can cause weakness or numbness in the arms or legs. In some areas, such as the thalamus, they can also cause pain. A cavernous malformation in the brainstem can cause coordination problems called ataxia or can cause facial paralysis, usually on one side.
- Cavernous malformations can cause vision problems. There are two kinds of vision problems: those caused by lesions in the occipital lobe of the brain, which affect how visual information is processed, and those caused by lesions in the brainstem, which affect how the eyes work.
- A cavernous malformation can cause hearing problems, including loss of hearing and tinnitus, dizziness, or nausea, particularly if it is located in or near the cerebellum.
- A cavernous malformation in the medulla, the lowest part of the brainstem, can cause spasms of the diaphragm, which resemble hiccups that don’t go away. More rarely, these can cause swallowing or even breathing problems.
- Cavernous malformation hemorrhages in the brain can cause fatigue. Individuals may complain of fatigue for months to years after a major hemorrhage or brain surgery.
- Spinal cord cavernous malformations can cause numbness, weakness, paralysis, tingling, burning, or itching. The location and extent of the symptom depend on the level of the spine affected. Spinal cord lesions can also cause difficulty with bladder and bowel control.

PATIENT STORY: Joyce
Spinal Cavernous Malformation
“I had just put my left arm down on the kitchen table when I experienced this intense pain from the tips of my fingers to my elbow,” Joyce told the New York Times in a 2007 interview. “It felt like my whole arm was burning.”
It would be years before doctors accurately diagnosed Joyce with a cavernous malformation in her cervical spinal cord. By that time, the pain had spread to her right arm. Her surgeon told her the lesion was accessible, and Joyce had successful surgery in 2004. The surgery helped to resolve some of Joyce’s pain and to prevent any further escalation.
Joyce also has multiple cavernous malformations in her brain. This is because of a hereditary genetic change known as the Common Hispanic Mutation. While anyone can have a hereditary form of cavernous malformation, thousands of people who trace their heritage to the original Spanish settlers of New Mexico share this specific genetic mutation. A single ancestor connects them all, and many of these families have remained in New Mexico, including Joyce. No other place in the world has as many affected people.
Joyce has been active in advocacy and in raising awareness of the illness throughout New Mexico. In addition to the New York Times interview, Joyce was central in drafting legislation in New Mexico that created a mandate to educate more doctors. Joyce has presented at patient conferences and worked with media around the state to share her story and the genealogy she has researched.
Joyce was happy to discover that neither of her children inherited the illness. In Joyce’s family, the Common Hispanic Mutation has stopped with her, though her work toward further research and a cure continues.
9) HOW OFTEN DO I NEED AN MRI?
You and your doctor will decide how often to repeat your MRI. Some doctors advise their patients to obtain repeat MRIs on a specific schedule. Others suggest waiting until there are additional symptoms Experts suggest more frequent imaging for those who may not be able to report symptoms, like young children or those with intellectual or communication problems. These individuals may also need sedation for MRI. You and your doctor will weigh the risk of sedation against the benefit of imaging. CT scan is another kind of imaging that is sometimes used. CT scan is much faster than MRI, but the images are not as clear, and the CT scan involves exposing a patient to radiation. You may have a CT scan in an emergency when MRI is not available. People with multiple cavernous malformations should limit their exposure to CT scans as much as possible because it is not clear whether the radiation exposure can cause the development of more lesions. A doctor may suggest a cerebral angiogram also known as a cerebral arteriogram. This procedure allows the doctor to see the arteries and veins in your brain. A cavernous malformation is not visible on an angiogram, but the test is done when another type of blood vessel lesion, called an arteriovenous malformation, is suspected. If a cavernous malformation has a typical appearance on MRI, it does not require a cerebral angiogram as part of routine care.
10) DO I NEED SURGERY?
If your cavernous malformation (cavernous angioma, cavernoma) is causing symptoms, you should have a very detailed discussion about surgical options with your neurosurgeon. The decision to have surgery always involves weighing risks and benefits. In general, experts recommend surgery if three criteria are met. First, the individual must have symptoms. Second, the cavernous malformation must have had at least two hemorrhages. Finally, removing the cavernous malformation will cause fewer deficits than another hemorrhage would. Sometimes, experts recommend surgery after just one hemorrhage. For example, surgery may be a good option for someone with epilepsy caused by a cavernous malformation even if they have only had one hemorrhage.
There are neurosurgeons who specialize in cerebrovascular (brain blood vessel) and skull base (brainstem) surgery. The experience level of a surgeon is the best predictor of a good surgical outcome. The American Academy of Neurological Surgeons offers a searchable directory of neurosurgeons by specialty. It is helpful to interview a number of surgeons, including asking them about their experience, and to consult with other patients through Alliance to Cure Cavernous Malformation before making decisions.
11) ARE OTHER TREATMENTS FOR CAVERNOUS malformation (Cavernous angioma, cavernoma) AVAILABLE?
Doctors have treated cavernous malformation with stereotactic radiosurgery, also known as gamma knife, linear accelerator, X Knife, Brainlab, or cyberknife, for many years, but its effectiveness is not clear. In stereotactic radiosurgery, focused radiation is directed at the cavernous malformation without opening the skull. Experts now recommend that radiosurgery be considered only with individuals who have a single symptomatic lesion that is in an area of the brain where the risks of traditional surgery would be too high. Radiosurgery should not be used for treating cavernous malformations that do not cause symptoms or for cavernous malformation in people with the hereditary form of the illness, as the radiation itself might trigger new cavernous malformations to form. Other minimally invasive surgical techniques are being used more widely.
Researchers are working to find medications to treat cavernous malformations. It may take more than one medication to treat every situation. Medications could be useful to:
- Stabilize the cavernous malformation so it does not hemorrhage. Patients could use medications even before a first hemorrhage. This is particularly true for people with hereditary forms of the illness.
- Stabilize the cavernous malformation after a hemorrhage to reduce the risk of the lesion bleeding again. Remember, there is a high-risk time in the first years after a hemorrhage. During this time, it might make sense to use a stronger temporary medication.
- Slow or stop the development of more lesions in people who have multiple cavernous malformations.
- Shrink or destroy existing cavernous malformations. This is the ultimate goal.
12) DO I NEED GENETIC TESTING?
Most people with a cavernous malformation do not need genetic testing. We believe only 20-25% of individuals with a cavernous malformation have a hereditary form of the illness. If you have just one cavernous malformation, you need an MRI with special imaging called susceptibility-weighted imaging (SWI) to rule out the hereditary form. If you have multiple cavernous malformations but you also have a developmental venous anomaly (DVA), SWI will show whether your lesions cluster near the DVA or whether they are in other areas of your brain. If the cavernous malformations are only around the DVA, you do not need testing. Having multiple cavernous malformations clustered around a DVA is typical of the sporadic form of cavernous malformation. You can’t inherit or pass down the sporadic form of the illness. People who have multiple cavernous malformations that are not associated with a developmental venous anomaly should request genetic testing. Sometimes people are the first in their family with a hereditary form. You do not need other affected family members to justify testing.
13) WHICH GENES WILL THE LABORATORY TEST?
There are three known genes that, when mutated, can cause a hereditary form of the illness. Researchers have named them CCM1, CCM2, and CCM3. In the United States, individuals who trace their ancestry to the original settlers of New Mexico and Chihuahua, Mexico have passed a specific mutation of the CCM1 gene down from generation to generation since at least the early 1600s. Researchers call this the common Hispanic mutation. However, you do not need to be Hispanic to have the hereditary form of the illness. Hereditary forms of cavernous malformation exist in every ethnic group everywhere in the world.
Each child of a person with the hereditary form has a 50/50 chance of inheriting the illness. It does not skip generations. However, up to half of the people with a hereditary form may have lesions but have no symptoms. Individuals with a mutation of the CCM1 or CCM2 gene develop multiple cavernous malformations and some develop cavernous malformations under the skin.
Individuals with a mutation on the CCM3 gene may have additional features. About half of individuals with a mutation on the CCM3 gene have their first hemorrhage as children. They hemorrhage more often and develop new lesions more quickly, at a rate of 2-3 new lesions per year (compared to an average of one lesion every two years for those with CCM1 or CCM2 mutations). They may have other physical issues such as scoliosis and benign brain tumors, most commonly meningioma. They are also likely to be the first in their family with the illness. Patients with a CCM3 mutation need additional monitoring and should contact Alliance to Cure Cavernous Malformation to learn more about our special programs.
14) HOW DO I GET GENETIC TESTING?
A medical professional such as a neurologist, neurosurgeon, geneticist, or genetic counselor must order genetic testing. Only a few labs in the United States perform testing, and many insurance companies do not cover the expense. Our website contains a list of testing laboratories and information about our free genetic testing program for individuals who qualify. Depending on the laboratory, you will submit either a blood or a saliva sample for testing. It may take up to six weeks to receive results. After you have received your result, your doctor or genetic counselor can talk with you about genetic testing for other family members. This can be a difficult topic for extended families, and it is important to have the support of a health professional. Family members who are not experiencing symptoms may choose not to be tested or have their asymptomatic children tested. Genetic testing is a very personal decision.
 Patient Story: Vern
Patient Story: Vern
DVA with Cavernous Malformation
In 2004, Vern, then a 28-year-old father of two, hit his head while practicing jujitsu. From the subsequent CT scan, Vern and his wife Tiffany were surprised to learn that Vern had a more serious and long-term condition. Doctors diagnosed him with multiple cavernous malformations (cavernous malformations, cavernoma) surrounding a large developmental venous anomaly (DVA), a dilated malformed vein, in his brainstem. While a DVA by itself typically does not cause symptoms or complications, Vern’s DVA had set the stage for the development of more than one cavernous malformation.
It was not until two years later that Vern had his first hemorrhage. As a result, he closed his business as a mobile fleet service mechanic to focus on his recovery and his family. “I couldn’t drive,” Vern explains. “My reaction time was just not near what it needed to be to operate a vehicle safely.” Vern is driving again, but not on interstates or during times of heavy traffic. He also has been recovering from gait and vision deficits.
Vern has consulted numerous surgeons about removing the most problematic of his cavernous malformations. The DVA complicates surgery. Vern’s wife Tiffany explains, “The angioma that keeps bleeding is located too close to his DVA to remove. The DVA looks almost like a hook, and the angioma is on the inside of that hook.” Disturbing a large DVA like Vern’s can cause a catastrophic stroke.
Tiffany continues, “Vern has learned that being busy and doing something productive each day makes a huge difference in his quality of life. Vern has always had a very active lifestyle, but since having his bleeds, he has learned how to do things safer and smarter. He follows what doctors have told him to do and not to do… well mostly. All in all, Vern’s doing well.”
15) SHOULD I HAVE CONCERNS ABOUT PREGNANCY WITH A CAVERNOUS malformation (cavernous angioma, cavernoma)?
At this time, experts believe women are no more at risk for hemorrhage during pregnancy than at any other time. But, a bleed during pregnancy can present challenges. Brain surgery to remove a cavernous malformation (cavernous angioma, cavernoma) during pregnancy is very rare but is undertaken in cases where a second hemorrhage would be life-threatening. Women with cavernous malformations can have a vaginal delivery if they have not had a recent hemorrhage. If your doctor suggests an MRI during your pregnancy, your MRI should not include gadolinium contrast. Women who have epilepsy and are on anti-epilepsy medications should talk with their doctors about the choice of medication and folate supplementation. Ideally, you should have this conversation before you become pregnant to prevent harm because some antiepilepsy medication can increase the risk of birth defects when taken in the first weeks of pregnancy. However, having a seizure during pregnancy can cause harm that is far more serious to the fetus. It’s important to continue antiepilepsy medication during pregnancy if you have had seizures and are pregnant.
16) ARE THERE SPECIAL ISSUES FOR CHILDREN WITH A CAVERNOUS malformation?
There is the potential for many special issues with children, depending on their age at diagnosis and their symptoms. Young children may not be able to tell you about symptoms, so it becomes important to schedule imaging regularly. On the other hand, it is also important to avoid overreacting so that children aren’t exposed to unnecessary medical procedures, radiation from CT scans, MRI contrast medication, and sedation. It is not always possible to strike a balance, and every parent will err in both directions at one point or another. As a child grows older and parents become more experienced, managing this illness becomes easier. Telling your child about his or her diagnosis can be emotional and can require a period of adjustment for your child. Try to explain in simple terms that are age-appropriate. Having a pediatric mental health professional ready to help can make this easier. A mental health professional can also help if a child with hemorrhage or surgery-related deficits struggles with peer relationships, restrictions on activities, or academics. You will need to explain your child’s illness many times to many professionals including school staff, as well as friends and other caregivers. Good support from other parents in the Alliance to Cure Cavernous Malformation community or your local special needs community can be helpful for you.
17) WHAT SHOULD I ASK MY DOCTOR?
If you don’t already know the answers to these questions, you may want to ask these at your next appointment and write the answers here.
- WHAT SIZE IS THE CAVERNOUS MALFORMATION (CAVERNOUS ANGIOMA, CAVERNOMA)?
- HOW MANY CAVERNOUS MALFORMATIONS DO I HAVE?
- WHAT IS THE EXACT LOCATION OF THE CAVERNOUS MALFORMATION?
- WHAT FUNCTIONS DOES THIS AREA OF THE BRAIN CONTROL?
- DO THERE APPEAR TO BE ANY VENOUS OR OTHER MALFORMATIONS NEAR THE CAVERNOUS MALFORMATION?
- DOES IT APPEAR TO HAVE BLED PREVIOUSLY?
- IN YOUR OPINION, WHAT ARE THE CONDITIONS UNDER WHICH YOU RECOMMEND SURGERY TO REMOVE THIS CAVERNOUS MALFORMATION?
- IF I HAVE ANOTHER BLEED, WHAT SYMPTOMS WOULD YOU EXPECT?
Please also consult our additional questions to ask your doctor about specific situations, like surgery.
18) HOW DO I COPE?
Receiving a diagnosis of cavernous malformation (cavernous angioma, cavernoma) in the brain or spinal cord for you or a loved one can be difficult and upsetting. No matter your level of medical involvement, you will require a period of adjustment to a “new normal” which will include a time of grieving for what has changed. A counselor or other mental health professional can help if you experience emotional difficulty that interferes with your ability to get through your days. Close friends and family may have difficulty understanding, particularly if you don’t appear ill. The Alliance to Cure Cavernous Malformation online community or one-on-one peer support can be helpful as you look for others who share your issues.
19) ARE THERE OTHER WAYS I CAN BE SAFER?
Request a CD with your most recent MRI and a printed copy of the radiology report. This is good to have with you when you travel and in case of an emergency. You may also want to wear a medical alert bracelet indicating you have a condition that can cause a brain hemorrhage. Finally, you can have your medical information in more detail on your cellphone. Some cellphones offer apps that emergency personnel can access even when your phone is locked.
20) WHAT DOES ALLIANCE TO CURE OFFER PATIENTS AND FAMILIES?
Our mission is to inform, support, and empower those affected by cavernous malformation (cavernous angioma, cavernoma) and drive research for better treatments and a cure.
PATIENT INFORMATION: Alliance to Cure Cavernous Malformation provides extensive information on our website and in our newsletter. We announce new research findings as they are published. We host patient conferences with presentations by disease experts. You can view these at any time on our YouTube channel.
PATIENT SUPPORT: Alliance to Cure Cavernous Malformation offers patient support through Facebook, facilitated video conferences, and through our local Community Alliances. At our patient conferences, we offer time for attendees to share their stories.
GENETIC TESTING: Alliance to Cure Cavernous Malformation offers free genetic testing to individuals with multiple cavernous malformations who can’t get coverage through their insurance.
OPPORTUNITIES TO PARTICIPATE IN RESEARCH: Alliance to Cure Cavernous Malformation has a patient registry where you can sign up to be notified about research studies, including clinical drug trials, that are recruiting. We also are collaborators in multiple projects that are exploring the impact of the illness on patient’s quality of life.
CLINICAL CENTERS: Alliance to Cure Cavernous Malformation has a growing network of recognized Clinical Centers that provide expert multi-disciplinary care.
AWARENESS EVENTS: We sponsor volunteer-organized awareness opportunities around the country including community walks. In addition to these patient and family activities, Alliance to Cure Cavernous Malformation sponsors the annual International CCM Scientific Meeting, which brings together researchers from around the world. We provide consultations to assist with their clinical drug trial planning.
GOING FORWARD
A cavernous malformation diagnosis may seem overwhelming. Alliance to Cure Cavernous Malformation is an excellent resource for you and your family members to meet others and learn more. Even though the diagnosis is rare, our online patient and family communities are large and growing. We are committed to helping each other.
Updated 4.26.23

 Patient Story: Stacie
Patient Story: Stacie Patient Story: Taylor
Patient Story: Taylor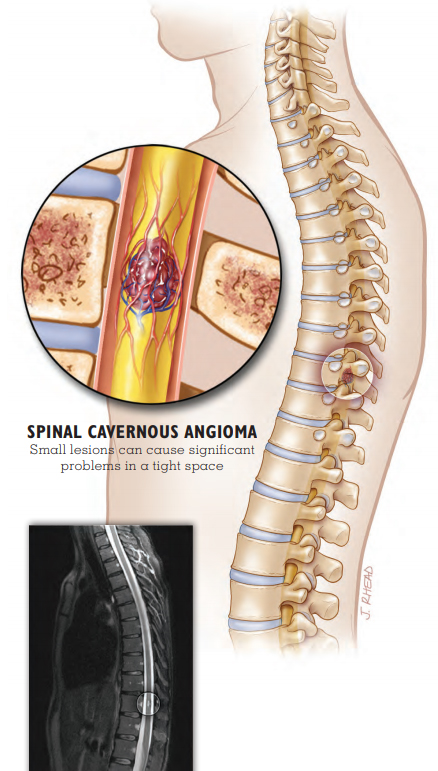
 Patient Story: Vern
Patient Story: Vern