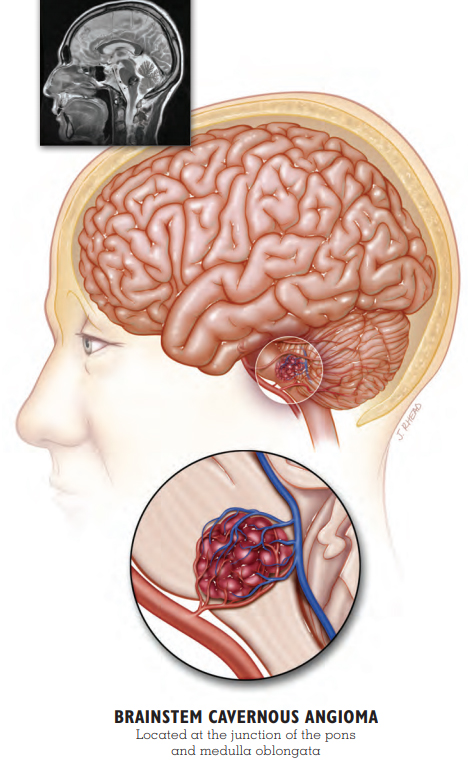
Why is this region so delicate?
The brainstem is a small region packed with nerve fibers that control voluntary and involuntary functions in the body, including regulation of heart rate, breathing, sleeping, and temperature. Damage to this area can cause more serious effects than other locations within the brain and is associated with greater morbidity and mortality.
Brainstem lesions by the numbers
- Approximately 20% of cavernous malformations are located in the brainstem.
- Studies have indicated that brainstem lesions are more likely to present with an initial hemorrhage and are more likely to rebleed. A paper published in 2020 (Flemming et al) found that brainstem location is a strong predictor of hemorrhage. In this study, brainstem hemorrhage location was most common in patients who presented with hemorrhage (58%).
- A study measured re-hemorrhaging rates as high as 30% per person. Other studies show varying rates of re-bleeding.
Symptoms
The most common symptoms for brainstem lesions are focal neurological deficits, as opposed to seizure or headache for lesions located in other regions of the brain. These focal neurological deficits can include:
- Coordination and movement challenges, or ataxia
- Speech and swallowing difficulties
- Facial paralysis (usually on one side)
- Vision and auditory problems
- Hiccups as a result of diaphragmatic spasms
- Breathing difficulties that can contribute to sleep issues, including sleep apnea
Management of brainstem cavernous malformation
The current recommendations for the management of brainstem lesions are outlined in the Clinical Care Guidelines. This is a great resource to share with your providers so that you can make the best decisions regarding your care.
Watch and wait (conservative management)
This approach is most often recommended, especially in lesions that have not bled or are asymptomatic. Conservative management consists of routine, periodic MRIs to monitor the changes in the lesion. As long as the lesion appears stable and there are no additional symptoms or evidence of hemorrhage, this is usually the most prudent course of action.
Surgical removal (resection)
Surgical removal should be considered on a case-by-case basis with the risks and benefits weighed. Surgery should be performed by a surgeon with CCM and skull-base surgery expertise. Surgical resection may be considered if the lesion is symptomatic and has bled on at least one occasion.
Stereotactic radiosurgery (gamma knife)
Radiosurgery is a non-surgical targeted treatment for CCM. According to the CCM clinical care guidelines, stereotactic radiosurgery should only be considered for solitary lesions that have previously hemorrhaged and carry a high surgical risk. It is not advisable to attempt radiosurgery on those with hereditary disease due to the risk of developing additional lesions following radiation.
Self-management through a positive lifestyle
While treatment options for brainstem lesions appear to be limited, new information is emerging about what is within your control in terms of lifestyle management and its impact on cavernous malformation.
Associated DVA
Developmental venous anomalies (DVA) are frequently associated with a cavernous malformation in the brainstem. According to a 2019 study (Kumar et al), DVA located in the brainstem has been shown to increase the risk of having a cavernous malformation by 2.6 times.
PATIENT STORY: TAYLOR
 Brainstem Cavernous Angioma
Brainstem Cavernous Angioma
In January 2015, three-year-old Taylor’s parents, Elizabeth and Pasco, grew concerned when they noticed changes in their daughter’s behavior. Taylor’s walking was unsteady, her speech was impaired, and her face was drooping. MRI confirmed that Taylor had a large cavernous malformation that had hemorrhaged in the pons region of her brainstem.
Taylor’s parents faced a difficult decision. Surgically removing the cavernous malformation could result in additional deficits. However, another hemorrhage could be life-threatening. Elizabeth and Pasco obtained multiple surgical opinions and decided to move forward with surgery at a hospital on the other side of the country.
Nine months after the onset of her symptoms, Taylor underwent the delicate operation. Taylor emerged from the surgery with left-sided facial paralysis, not uncommon with trauma to the pons. She had difficulty coordinating her movements, which affected her standing and walking.
Since her surgery, Taylor has undergone intensive physical rehabilitation and made great improvements in her ability to get around. Her family is researching options to bring movement back to her face.
Because she had additional cavernous malformations, Taylor received genetic testing. Testing revealed a mutation of the CCM3 gene, which tends to lead to a more severe form of cavernous malformation illness. Taylor is the first in her family to have a CCM3 mutation.
Taylor’s parents are grateful for the positive surgical outcome, but they still worry. “Unfortunately, always in the back of mine and her daddy’s mind is the anxiety of not knowing what is going on in there,” said Elizabeth. “Is there any new activity, anything we should know about?”
Elizabeth and Pasco treasure Taylor and her resilience. “She is beautiful, smart, charming, witty, stubborn, and strong. She still amazes us every day with things she does.”
Support
We offer support for brainstem patients and their loved ones through our private Facebook group or you may reach us at info@alliancetocure.org for more information.
Updated 4.16.22
References
-
Flemming KD, Kumar S, Brown RD Jr, Lanzino G. Predictors of Initial Presentation with Hemorrhage in Patients with Cavernous Malformations. World Neurosurg. 2020 Jan;133:e767-e773.
-
Kumar S, Lanzino G, Brinjikji W, Hocquard KW, Flemming KD. Infratentorial Developmental Venous Abnormalities and Inflammation Increase Odds of Sporadic Cavernous Malformation. J Stroke Cerebrovasc Dis. 2019;28(6):1662-1667.
-
Akers A, et al. Synopsis of guidelines for the clinical management of cerebral cavernous malformations: consensus recommendations based on systematic literature review by the Alliance to Cure Cavernous Malformation Scientific Advisory Board Clinical Experts Panel. Neurosurgery. 2017;80(5):665–680.

 Brainstem Cavernous Angioma
Brainstem Cavernous Angioma